Spirometry, Pulmonary
+++++++++++++++++++++++++++
Test used to assess how well the lungs function by measuring how much air is inhaled, how much is exhaled and how quickly it is exhaled.
-
Volumes or the ability of the lungs to fully expand (TLC, FRC, RV).
-
Flow rates or the rate of inflow and outflow of air (FEV1, forced expiratory flow [25%-75%]).
-
Maximum voluntary ventilation or airflow through major airways by rapid inspiration and expiration maneuvers (MVV).
-
Maximum inspiratory and expiratory pressure, a measure of respiratory muscle strength (Pi[max], Pe[max]).
-
Diffusing capacity (DLCO) or measurement of the ability of oxygen to get into the blood.
Interpretation will be (1) normal, (2) obstructive, (3) restrictive, or (4) combined obstructive and restrictive.
PFTs assesses the mechanical function of the respiratory system, to quantitate the loss of lung function, and to monitor disease progression and response to treatment.
PFTs also predict postoperative risk of pulmonary complications and which patients will likely have adequate pulmonary function after lung resection. Serial evaluations monitor respiratory muscular strength in progressive neuromuscular diseases such as Guillain-Barre, myasthesia gravis, and muscular dystrophy.
Spirometry is used to diagnose asthma, chronic obstructive pulmonary disease (COPD) and other conditions that affect breathing.
Spirometry may also be used periodically to monitor your lung condition and check whether a treatment for a chronic lung condition is helping.
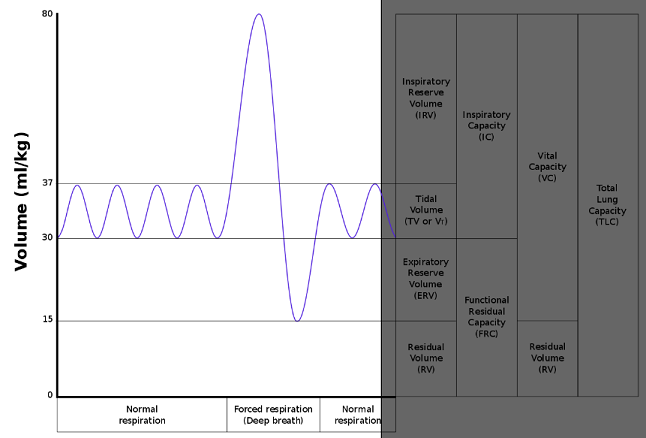
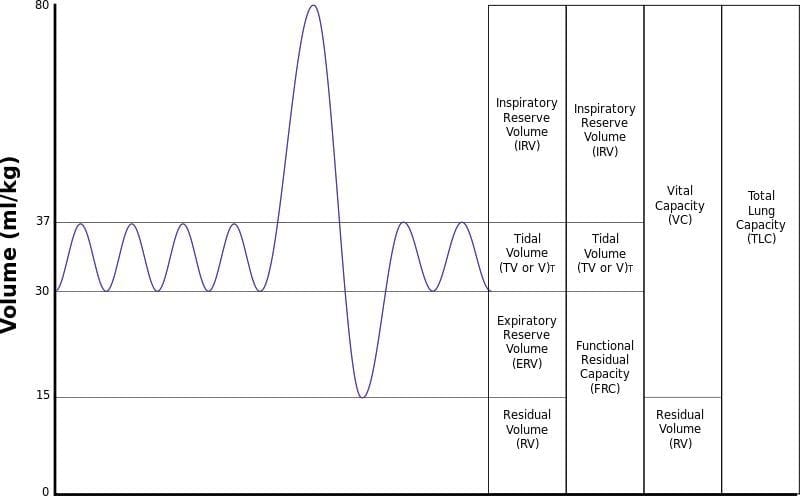
Spirometry of a normal person taking 4 tidal breaths, followed by maximal inspiration and expiration.
Corresponding volumes and capacities are noted in the right-hand boxes
Functional Residual Capacity(FRC) is the volume of air present in the lungs at the end of passive expiration. At FRC, the opposing elastic recoil forces of the lungs and chest wall are in equilibrium and there is no exertion by the diaphragm or other respiratory muscles.
FRC is the sum of Expiratory Reserve Volume (ERV) and Residual Volume (RV) and measures approximately 2400 mL in an 80 kg, average-sized male. It cannot be estimated through spirometry, since it includes the residual volume. In order to measure RV precisely, one would need to perform a test such as nitrogen washout, helium dilution or body plethysmography.
A lowered or elevated FRC is often an indication of some form of respiratory disease. For instance, in emphysema, FRC is increased, because the lungs are more compliant and the equilibrium between the inward recoil of the lungs and outward recoil of the chest wall is disturbed. As such, patients with emphysema often have noticeably broader chests due to the relatively unopposed outward recoil of the chest wall. Total lung capacity also increases, largely as a result of increased functional residual capacity. In healthy humans, FRC changes with body posture.
Obese patients will have a lower FRC in the supine position due to the added tissue weight opposing the outward recoil of the chest wall.
The helium dilution technique and pulmonary plethysmograph are two common ways of measuring the functional residual capacity of the lungs.
The predicted value of FRC was measured for large populations and published in several references.[1][2][3][4] FRC was found to vary by a patient's age, height, and sex.
An online calculator exists that will calculate FRC for a patient using these references.
Spirometry results indicate the presence of obstructive airway diseases such as asthma and emphysema when the FEV1/FVC ratio is < 0.70.
They indicate the presence of restrictive lung diseases such as sarcoidosis and ankylosing spondylitis when the FVC/FEV1 ratio > 80%.
Obtain spirograms before and after administration of bronchodilators if they are not contraindicated (ie, history of intolerance). Bronchodilator responsiveness helps in predicting the response to treatment and in identifying asthma. Asthmatic patients typically have at least 15% improvement in FEV1 after bronchodilator therapy.
Capacity = any combination of 2 or more volumes
LUNG VOLUMES
FLOW VOLUME LOOP
PARAMETERS
- VC = 70mL/kg
= IRV + TV + ERV - IRV = 45mL/kg
- TV = 10mL/kg – volume breathed in & out during a normal breath (without extra effort)
- ERV = 15mL/kg – extra volume beyond normal expiration
- RV = 15mL\kg (not measured by spirometer)
- TLC = 85L\kg
- FRC = 30mL\kg
- FEV1 = forced expiratory volume in 1 second (normally 4L)
- FVC = forced vital capacity (a little lower than VC because of dynamic airway closure; normally ~5L)
- PEFR = peak flow rate over an expiration (normally 500L/min)
- FEV1/FVC (normal = 80%)
– obstructive disease = FEV1 reduced more than FVC, low FEV1/FVC
– restrictive disease = FEV1 & FVC reduced but FEV1/FVC normal or increased
– after a relatively small amount of gas has been exhaled -> flow is limited by airway compression determined by (1) elastic recoil force of lung & (2) resistance of airways upstream of the collapse point. - FEF50%
- FIF50%
- FEF/FIF50 = if > 1 -> inspiratory flow is affected more than expiratory -> extrathoracic site of obstruction
OBSTRUCTIVE DISEASE
- flow rate very low in relation to lung volume (c/o resistance to flow – scooped out appearance often seen following the point of maximum flow)
- total lung capacity is large, but expiration ends prematurely c/o early airway closure from increased smooth muscle tone of bronchi (asthma) or loss of radial traction from surrounding parenchyma (emphysema).
- equal pressure point is close to the alveolus and the transmural pressure gradient can become negative quickly -> collapse.
- encroachment of VC by an increased RV caused by hyperinflation (‘air trapping’)
RESTRICTIVE DISEASE
- total volume exhaled and flow rate reduced
- inspiration limited by reduced compliance of lung/chest wall or weakness of inspiratory muscles